We have known for a while that most back surgeries don’t yield results significantly better than Physical Therapy in most cases. This is also true of shoulders and knees when trauma is not involved. But, surely patients need back surgery if the canal where the spinal cord travels is narrowed, a condition known as Spinal Stenosis. It is often seen after long standing Degenerative Arthritis which causes the inside of the vertebrae making up the spinal canal to grow narrower. Visualizing the spinal cord getting squeezed inside its bony sheath conjures thoughts of permanent nerve damage. Surely, this can’t be good, right?
Amazingly, some courageous doctors have shown that surgery for Spinal Stenosis is no better than Physical Therapy!
“Surgical decompression yielded similar effects to a PT regimen among patients with Lumbar Spinal Stenosis (LSS) who were surgical candidates. Patients and health care providers should engage in shared decision-making conversations that include full disclosure of evidence involving surgical and nonsurgical treatments for LSS.”[1]
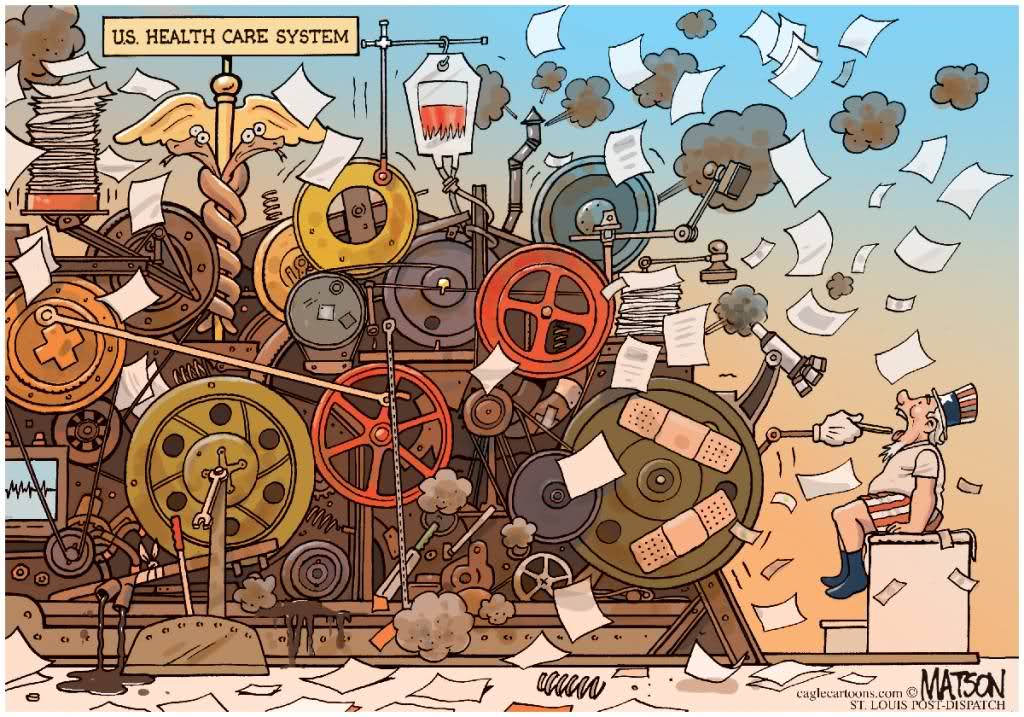
This is still useful information even though you may not have arthritic problem for which you have been told you need surgery. Think of it this way: we have created a Health Care System that needs to be fed… a lot.[2]
I am afraid that about 80% of surgeries could be avoided with a judicious, conservative approach involving a good diet, lifestyle changes and physical therapy, and/or chiropractics.
There will be a lot of push back against the article herein quoted and this editorial. Just follow the money.
Hugo Rodier, MD
BRAIN POWER
That is the title of Dr. Permutter’s new book on the Brain-Gut connection. He is a world-renown neurologist who works with non pharmaceutical treatments, mostly to prevent disease. I still think my book GUT HEALTH is better (Ha!) because it addresses more than the Brain-Gut connection, but the Gut connecting with ALL organs; thus, it covers how the gut determines health at the cellular level. Here is some more proof:
“Obese type gut microbiota induce neurobehavioral changes in the absence of obesity,”[3] The link between obesity, the microbiome and neurologic function-the brain gut connection
“Diet and Upper Gastrointestinal Malignancies,”[4]
“Nutrients, Foods, and Colorectal Cancer Prevention,”[5]
“Diet and Upper Gastrointestinal Malignancies,”[6]
“Nutrients, Foods, and Colorectal Cancer Prevention,”[7]
“Food, the Immune System, and the Gastrointestinal Tract,”[8]
“Diet in the Pathogenesis and Treatment of Inflammatory Bowel Diseases,”[9]
“Food Components and Irritable Bowel Syndrome,”[10]
“Food, Immunity, and the Microbiome,”[11] This one is worth quoting from:
“There is increasing evidence that ingested diet-borne components are involved in the pathogenesis of disorders such as inflammatory bowel diseases, atherosclerosis, and type 2 diabetes. Nutrients can have short- and long-term effects in shaping the composition of the microbiota. Western diets (enriched in fat, phosphatidylcholine, and L-carnitine) promote inflammation and atherosclerosis through specific fatty acids and degradation products such as trimethylamine N-oxide. Other dietary factors such as carbazoles or tryptophan-enriched proteins have anti-inflammatory properties—partly via activation of aryl hydrocarbon receptors. The microbiota and its metabolic machinery produce a myriad of metabolites that serve as important messengers between the diet, microbiota, and host. Short-chain fatty acids affect immune responses and epithelial integrity via G-protein–coupled receptors and epigenetic mechanisms. By increasing our understanding of interactions between diet, immunity, and the microbiota, we might develop food-based approaches to prevent or treat many diseases. There now is scientific evidence to support the adage “we are what we eat,” and this process begins in early life.”
“Microbial endocrinology: host–bacteria communication within the gut microbiome.” Your gut flora also affects hormone function:
“The human body is home to trillions of micro-organisms, which are increasingly being shown to have significant effects on a variety of disease states. Evidence exists that a bidirectional communication is taking place between us and our microbiome co-habitants, and that this dialogue is capable of influencing our health in a variety of ways. This review considers how host hormonal signals shape the microbiome, and what in return the microbiome residents may be signalling to their hosts.”[12]
Perhaps the most dramatic Gut connection is with the heart, as documented herein several times in the past. The article “Nonalcoholic Fatty Liver Disease and Vascular Function: Cross-Sectional Analysis in the Framingham Heart Study”[13] adds that there is an indirect effect from the gut flora to the heart and arteries: the liver. Given the epidemic of Fatty Liver we have in this country this should give us pause:
“For multiple measures of vascular function, the relationship with NAFLD (Fatty Liver) appeared largely determined by shared cardiometabolic risk factors. The persistent relationship with reduced peripheral arterial tonometry response beyond established risk factors suggests that NAFLD may contribute to microvascular dysfunction.”
In view of these articles, do you still feel safe taking acid blockers? They mess with your gut flora.[14] True, drugs like Prevacid and Nexium are often necessary if ulcers are involved, but most people end up on them due to indigestion caused by a poor diet. These drugs also block the absorption of minerals (osteoporosis association,) B vitamins, and the normal digestion of foods. Other than that they are just fine.
GREAT NEWS FOR MEN!
If you are a man you still remember the article in the JAMA published over 10 years ago about reducing your risk of prostate cancer by ejaculating more often. Here is an update from the recently concluded American Urology Academy Annual Meeting in New Orleans:[15] ejaculating 21 times a month reduces the risk of prostate cancer by 20%!
Your wife/SO may not be too happy to read this. Implementing this advice may involve some creativity, and PR skills. Good luck!
DIAGNOSING MENTAL ILLNESS
A basic understanding how ALL our body’s cells work[16] naturally leads to certain assumptions that more specific research invariably confirms. Such is the case with the different diagnoses of mental illness. For some time I have felt that the different mental illnesses, being treated with the same drugs in a “let’s-see-what-sticks” approach, share a common cellular root. If someone is diagnosed with Bipolar Disorder, or Depression, or Anxiety, or Shopping Disorder, etc., the differences in symptoms are often over emphasized and the similarities de- emphasized. While this may help in research for drugs or insurance billing, it lacks a more physiologic approach to recovery. Worse, it deprives the patient of a holistic understanding of the problem, and thus makes healing more pharmaceutical oriented.
This hypothesis is confirmed by a recent article, “Shared dimensions of performance and activation dysfunction in cognitive control in females with mood disorders.”[17] While it is true that each of us has genetic and behavioral tendencies that, given stress, poor relationships, bad diets, and other taxing life events, may cause us to behave in certain ways (thus the different diagnosis,) those stressors act upon our whole body, not just neurons. They lead to disease when the T.O.I.L.[18] they trigger impairs neuronal AND all cellular function.
Some patients do need medications, especially in time of crisis. But, to neglect the body of literature that shows nutrition and certain supplements are effective and safe is a disservice to our patients. In the past we have reviewed evidence to support the use of a plant based diet, exercise, counseling, massage and supplements like SAMe, folic acid MTHFR, omega oils, vitamins D & B, lithium orotate, and GABA.
LEFT OVER ARTICLES
“Air Pollution and Diabetes Risk: Assessing the Evidence to Date.” Environ Health PerspectMay 2015; DOI:10.1289/ehp.123-A134
“Associations between Long-Term Exposure to Chemical Constituents of Fine Particulate Matter (PM2.5) and Mortality in Medicare Enrollees in the Eastern United States,” Environ Health Perspect; PerspectMay 2015 DOI:10.1289/ehp.1307549
“Serum α->Tocopherol Has a Nonlinear Inverse Association with Periodontitis among US Adults.”
J. Nutr. 2015 145: 893
“Compared with Feeding Infants Breast Milk or Cow-Milk Formula, Soy Formula Feeding Does Not Affect Subsequent Reproductive Organ Size at 5 Years of Age.”
J. Nutr. 2015 145:871
“Association of coffee intake with total and cause-specific mortality in a Japanese population: the Japan Public Health Center–based Prospective Study.” Lower mortality with coffee
Am J Clin Nutr 2015 101: 1029
“Egg consumption and risk of incident type 2 diabetes in men: the Kuopio Ischaemic Heart Disease Risk Factor Study.” Less DM with eggs.
Am J Clin Nutr 2015 101: 1088-1096; First published online April 1, 2
- “Surgery Versus Nonsurgical Treatment of Lumbar Spinal Stenosis: A Randomized Trial,” J.Ann Intern Med. 2015;162(7):465 ↑
- “Health Care 2020: reingeneering health care to combat chronic disease,” Am J. Med 2015;128:337“
Too much medicine ,” BMJ 2015; 350 :h1217 ↑ - J. Biol Psy 2015;77:607 ↑
- J. Gastroenterology May 2015 Volume 148, Issue 6, Pages 1234–1243.e4 ↑
- J. Gastroenterology May 2015 Volume 148, Issue 6, Pages 1244–1260.e16 ↑
- J. Gastroenterology May 2015 Volume 148, Issue 6, Pages 1234–1243.e4 ↑
- J. Gastroenterology May 2015 Volume 148, Issue 6, Pages 1244–1260.e16 ↑
- J. Gastroenterology May 2015 Volume 148, Issue 6, Pages 1083–1086 ↑
- J. Gastroenterology May 2015 Volume 148, Issue 6, Pages 1087–1106 ↑
- J. Gastroenterology May 2015 Volume 148, Issue 6, Pages 1158–1174.e4 ↑
- J. Gastroenterology May 2015 Volume 148, Issue 6, Pages 1107–1119 ↑
- J Endocrinol. 2015 May;225(2):R21-R34 ↑
- J. Arterioscler Thromb Vasc Biol. 2015;35:1284 ↑
- “Continuous Proton Pump Inhibitor Therapy and the Associated Risk of Recurrent Clostridium difficile Infection,” JAMA Intern Med. 2015;175(5):784 ↑
- Abstract PD6-07 Presented May 15 2015 ↑
- Watch my class online: www.hugorodier.com ↑
- J. Brain Epub 28 March 2015 ↑
- Toxicity, Oxidation, Inflammation, Less than optimal Mitochondrial function ↑


