Sweden did not do anything about the virus. Their mortality is now 30% higher than America’s.
Physical distancing measures may reduce spread of coronavirus, study indicates
CNN (7/16, Kane) reports “physical distancing measures can help slow down the spread of the novel coronavirus,” according to a study published in the BMJ. The study’s authors “gathered and analyzed information on daily reported cases from 149 countries or regions both before and after five different physical or social distancing measures were put into place.”
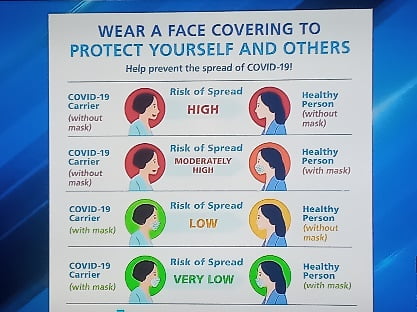
CDC calls for all Americans to wear face masks in public to combat coronavirus
CNN (7/14, Fox) reports, “The science shows face masks work both to protect the wearer and to protect others from coronavirus, and everyone needs to wear one when around other people in public, the Centers for Disease Control and Prevention said Tuesday.” CNN adds, “Even cloth face masks help enough to be worthwhile, three top CDC officials said in a commentary published in the Journal of the American Medical Association.” In the joint-editorial, “CDC Director Dr. Robert Redfield, CDC’s chief medical officer Dr. John Brooks and Deputy Director for Infectious Diseases Dr. Jay Butler” said, “While community use of face coverings has increased substantially, particularly in jurisdictions with mandatory orders, resistance continues.” The Hill (7/14, Moreno) reports, “The decision came after reviewing two studies: a JAMA study that found adherence to universal mask-wearing policies reduced transmission within a Boston hospital system, and an internal study from the CDC that found wearing a mask prevented the spread of infection from two hair stylists to their customers in Missouri.”
Utah Hospitals are on the brink of being overwhelmed
Salt Lake Tribune, July 13th 2020. ROBERT GEHRKE
“The chief medical officers from Utah’s four largest hospital chains issued a dire warning last week — unless things change significantly and soon, their intensive care units will be overwhelmed by COVID-19 patients.
“At this point I don’t think we can avoid maximizing our hospital capacity,” said Dr. Arlen Jarrett of Steward Health Care. “It seems clear we’re going to be maxing out our hospitals. I think it’s too late to make that change.”
Statewide, intensive care units are more than 72% full. In the Intermountain Healthcare system, 77% of beds hold a patient — even as the doctors agreed that the state’s current reporting system does not reflect what is really going on in the ICUs. Not long after the doctors spoke, the state announced 867 new cases of COVID-19, shattering Utah’s single-day record, and another 632 on Saturday. The Utah Department of Health reported 629 new cases Sunday.
The numbers make you shake your head, but Dr. Thomas Miller, chief medical officer at University of Utah Health, said what baffles him is that state leaders are not doing more to lower them.
“What’s a little difficult for me to understand as a physician who sees firsthand the toll this virus is taking on our health systems is why, as a state, haven’t we taken action to come together in a way we know will actually make a difference?” he said.
Dr. Mark Briesacher of Intermountain Healthcare said the doctors were sounding a hurricane warning and people need to act immediately.
These doctors joined a chorus of business leaders, medical professionals and faith leaders— which The Church of Jesus Christ of Latter-day Saints joined Friday— urging Utahns to wear masks to stop the spread of the virus. Most of them want Gov. Gary Herbert to make mask-wearing mandatory, which he has the power to do.
The governor, however, appears to be afraid of getting rolled by the Legislature. House Speaker Brad Wilson and Senate President Stuart Adams said in a statement that they oppose a mask mandate and the Legislature could, in theory, overturn a mandate from the governor.
So Herbert caved. Instead of requiring masks in high-risk counties, he once again asked Utahns to do the right thing for the right reason— a plea that has clearly not worked any time in the past six weeks.
And he “challenged” Utahns to get the number of new cases down to an average of 500 a day by month’s end, while doing nothing to make that goal possible.
We have not, since this pandemic began, seen a sustained decline in cases. Sure, cases were growing more slowly in March and April, but that was before Utah’s free-forall triggered explosive spread and made it the 22nd worst COVID-19 hot spot on the planet.
At the current rate of growth, Utah is on track to have nearly 20,000 new cases by the end of July. And if the governor acts on a mask requirement then, we’ll see another 19,000 in the two weeks before we start to see the impact.
It will push our medical system to the breaking point. There are plans to add emergency beds, but as Briesacher said, “Hospital beds and ICU beds don’t take care of people. It’s the nurses … the physicians, the pharmacists, they take care of people, and there is a limited number of those.”
What struck me the most about the call for action was a comment from Dr. Edward Stenehjem, with Intermountain, who said people don’t appreciate the toll COVID-19 takes on patients and their doctors and nurses, because it’s invisible.
“I really wish … I could take people into the hospital and walk through the ICU and listen to the ventilators and all the beeps and talk to our health care professionals who care for these people, and talk to the patients and realize how scared they are.”
He’d want to show them the husband and wife in intensive care who were put in rooms next door to each other in hopes the proximity would give them some comfort.
“Just walking the halls and talking to the patients and talking to our caregivers and understanding how tired they are and how scared they are would change anybody’s mind,” Stenehjem said.
There have been stories told of patients, knowing if they are put on a ventilator they may well never come off. Stories of doctors and nurses exhausted and emotionally drained. But perhaps we haven’t seen enough to snap some segment of the population into reality (a note on that at the end of this rant).
Intermountain Medical Center has an entire ICU full of COVID-19 patients, Stenehjem told me, something he has never seen before from one disease. Three or four patients are on machines— a last-ditch effort to keep a patient alive — that remove their blood, oxygenate it, and then return it to their bodies because their lungs are unable to do it.
On the sixth floor is award of less-critical COVID-19 patients, and they are alone.
“They suffer by themselves without the support of their families, so you can imagine what that does to a patient,” Stenehjem said. “It’s just tragic.”
Doctors and nurses are working long hours in protective equipment and a helmet with breathing equipment called a PAPR to keep them from inhaling the virus. They are worn down, Stenehjem said, and they too are afraid.
“It has taken a huge toll on people,” Stenehjem said. “It’s really hard. And it’s hard now and we’re just looking forward to it getting worse and I think that’s even more stressful, that unknown of what’s going to happen as we watch our peers in Arizona and Florida and Texas and New York City going through what we’re likely on the track to go through ourselves.”
That’s what we’re up against. Given the lack of courage and leadership from the governor on down, we’re going to be the ones who have to make the change, or else we’ll be the ones to suffer the consequences.”


